X+Y Scheduling
We follow a “3+1” model – instead of a typical 4-week rotation with one half day of continuity clinic per week, rotations occur in 3-week blocks (“X”) and are followed by one continuity clinic week (“Y”). During this “Y” clinic week, residents complete five half-days of continuity clinic, one half-day of large-group didactics on Thursday mornings (see below for more information!), one half-day of small-group outpatient didactics on Friday afternoons (see below for more information!), and can use the remaining three half-days for work on longitudinal curriculum assignments, QI/research projects, mentor meetings, personal appointments, and other educational experiences.
This scheduling model allows residents to be immersed completely in their rotation and focus entirely on their current experience. It also decreases the number of patient handoffs and improves continuity of care.
In the clinic, residents know their schedule for the entire year and can take charge of their own continuity; having clinic every fourth week allows for regular follow-up for each resident’s patient panel.
Our program has a substantial focus on wellness, and the X+Y scheduling model allows increased flexibility, consistent weeks with outpatient hours, and interval opportunities to attend personal appointments, greatly contributing to our residents’ wellbeing.
Thursday Morning Large Group Didactics
Most required conferences are clustered into a single weekly “Teaching Morning,” each Thursday from 8:00 a.m. to 1:00 p.m. This is time protected from clinical responsibilities so that you can focus on your education! These mornings include some very unique teaching series, and we are always trying new ways to learn:
- Pediatric Grand Rounds: Thursdays 8:00 AM – 9:00 a.m. Location: University of Michigan Health-Sparrow Hospital (Auditorium)
- Journal Club: Residents engage in discussion of a recent significant article. Principles of evidence-based medicine and critical appraisal of the medical literature are reviewed. Faculty will supervise the selection of articles and guide the scientific discussion.
- Subspecialty Cases: Residents, under the direct guidance of attendings, present interesting floor cases, PICU cases and NICU cases on a rotating basis. Residents and attending engage in discussion of up to date pediatrics as it relates to each case. These cases also allow for review and reflection of diagnosis and management for quality improvement and patient safety.
- Morbidity and Mortality: Residents, Fellows or Attendings present important cases of morbidity, including health care quality or patient safety issues, to facilitate identification of systems improvement opportunities and to address issues leading to medical error.
- Core Curriculum Conference: This series includes didactic sessions and group educational formats. It covers fundamental clinical, scientific and board specific topics based on the American Board of Pediatric Content Specifications, also including (but not limited to) important topics such as LGBTQ+ workshops, wellness/mindfulness, implicit bias and health equity, teaching medical students, and quality improvement.
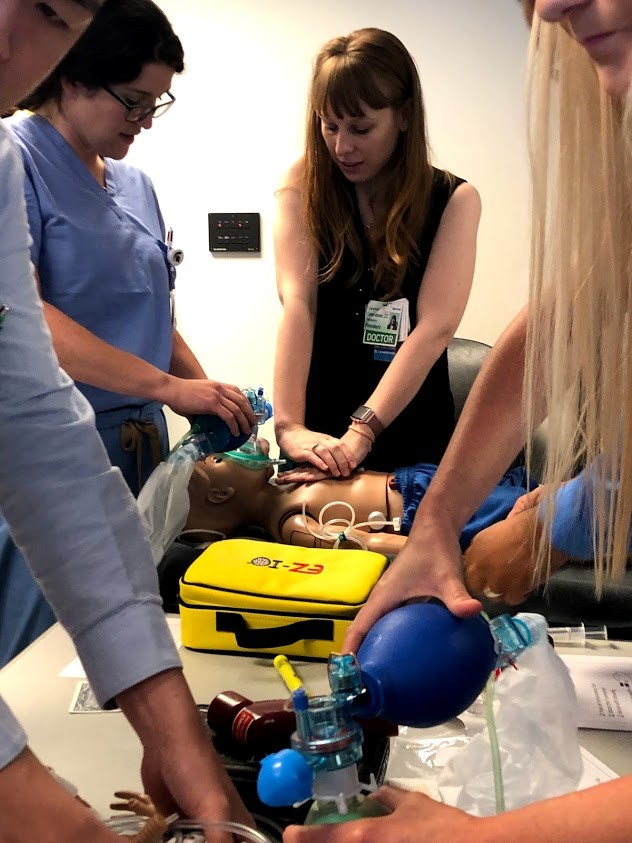
- Mock Code Simulation Curriculum: This series is led by pediatric intensivists once monthly on Thursdays with several different types of cases and scenarios to encourage skills practice.
- Wellness Series: This series occurs once monthly with a different fun activity or event or snack provided by the Pediatric Residency Wellness Committee with the support of the institutional GME office. We also have two half-day resident retreats during the year to focus on teambuilding and wellness.
- Chief and Program Leadership Check-Ins: These occur quarterly to allow for feedback on rotations and for our leadership team to provide support to residents.
Friday Afternoon Small Group Didactics
During the “Y” week, we have Friday afternoon outpatient didactics. All residents scheduled in clinic during that week do not have any patients scheduled and instead participate in small group didactics from 1:00 PM to 4:00 PM on Friday afternoons during their clinic week. These small group didactics involve case-based discussions regarding outpatient primary care scenarios, regular board review questions, program director check-ins, career planning, and other educational opportunities.
Scholarly Activity

Over the three years, residents are required to do a scholarly project of their choice in addition to an advocacy project (see below). This can be clinical or laboratory-based research or a quality improvement project. There is longitudinal time during your “Y” week dedicated to scholarly activity. Many residents have gone on to publish or present their projects nationally.
Child Advocacy Curriculum
Advocacy and community pediatrics have always been a focus at our program. Our advocacy curriculum is a longitudinal curriculum over three years of residency and includes didactics, experiential components/workshops, and an advocacy project to be presented at the end of the third year. There is dedicated time during your “Y” week to engage in your advocacy curriculum. Projects can be completed by individual residents or in groups. Didactic experiences occur during the scheduled resident teaching morning and include introduction to advocacy and community pediatrics, the medical home concept as well as other systems of care. Experiential components are primarily integrated into other rotations, namely the general pediatrics rotation and the developmental/behavioral pediatrics rotation. These experiences include home visits with maternal-infant health nurses, school visits, participation in evaluations of children with special needs, and participating in a child abuse evaluation. The primary workshop experience is the legislative advocacy experience. Taking advantage of our proximity to the state Capitol (home to the Michigan chapter of the American Academy of Pediatrics), we have instituted an annual experience that gives residents practice researching and developing a position paper, creating a fact sheet for legislators, and calling and meeting with legislators and their staffers.
Resident Wellness
Wellness is one of our program’s primary values. The Pediatric Residency Wellness Committee is a resident-led initiative that is program-supported. The work done by this committee has been presented regionally and nationally as cutting-edge examples of supporting resident wellness. One of our three Chief Residents is dedicated to wellness and our residents actively participate on the Sparrow Graduate Medical Education Wellness Committee which also provides different avenues of support for residents. For example, Sparrow Hospital has a Zero Barriers program which provides a psychiatrist on-call for residents and fellows with access to confidential mental health treatment and counseling.
Diversity and Inclusion
We pride ourselves on the diversity of our patient population, our faculty, and our residents. We strive to maintain an inclusive and supportive environment for all. We deliver multiple large and small group didactic experiences and workshops regarding this topic.
University of Michigan Health-Sparrow Hospital sponsors a Diversity, Equity, Inclusion, & Belonging Department which provides multiple caregiver resources including support groups such as “ABLE (Persons with Disabilities”, “Pride LGBTQIA+ & Allies”, “Military Network” and “Women in STEM & Allies”. University of Michigan Health-Sparrow also hosts a DEI Steering Committee, Racial Diversity Leadership Acceleration Program, and Women in Leadership Program.